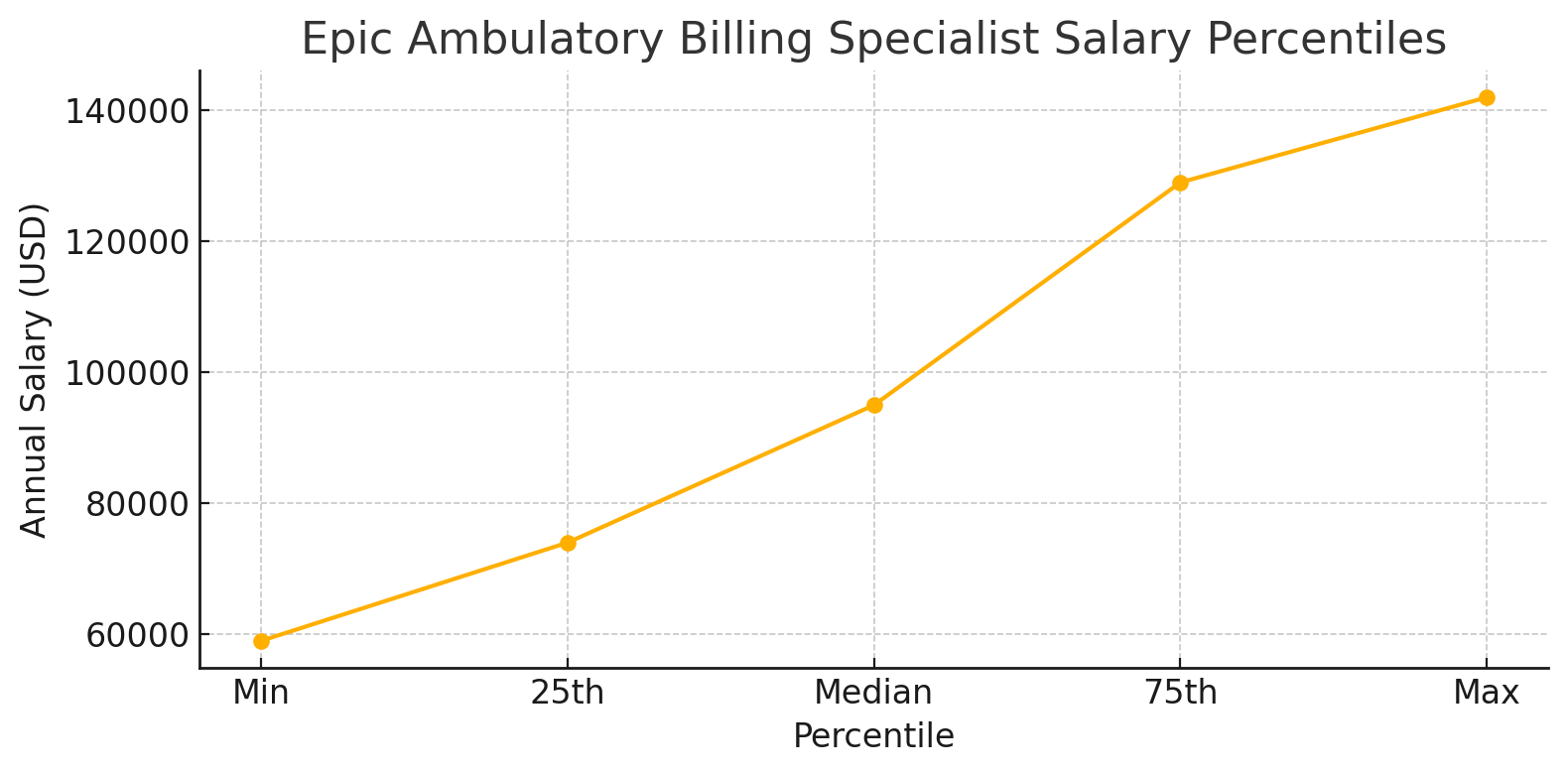
Epic Ambulatory Billing Certification prepares healthcare professionals to manage billing workflows in doctor’s offices and clinics that use Epic software. This certification teaches you how to process patient payments, submit insurance claims, and track billing information using Epic’s ambulatory (outpatient) platform. Getting certified shows employers you know how to handle the financial side of patient care outside the hospital. important thing is you will get huge hike on your salary. check the chart below!
Epic Ambulatory Billing Certification salary chart
What is Epic Ambulatory Billing Certification?
Certification Basics
Epic Ambulatory Billing Certification is a specialized credential for healthcare professionals who work with Epic’s outpatient billing system. Unlike general medical billing certifications, this one focuses specifically on how to use Epic’s software for managing charges, claims, and payments in clinic settings.
The certification verifies that you understand:
- How to navigate Epic’s billing modules for outpatient care
- The proper ways to enter charges and create claims
- Methods for tracking and resolving billing issues
- Procedures for posting payments correctly
- Best practices for maintaining clean revenue cycles
Why This Certification Matters
Healthcare organizations invest millions of dollars in Epic systems and need staff who can use them correctly. Having this certification:
- Shows employers you have specialized knowledge
- Reduces training time for new employees
- Helps ensure accurate billing and maximum revenue
- Decreases billing errors and rejected claims
- Improves overall financial performance for clinics
For healthcare workers, the certification can lead to better job opportunities and higher pay. Many job listings specifically request Epic certifications, making them valuable credentials in the healthcare job market.
The Path to Certification
Prerequisites and Requirements
Before you can pursue Epic Ambulatory Billing Certification, you need to meet certain requirements:
- Sponsorship: You must be sponsored by an organization that uses Epic. This is usually your employer.
- Role Qualification: You need to work in a position related to ambulatory billing or revenue cycle management.
- Basic Epic Knowledge: Some familiarity with Epic’s general interface is helpful but not always required.
- Education: While not strictly required, most successful candidates have education in healthcare administration, medical billing, or a related field.
Unlike some certifications that anyone can sign up for, Epic carefully controls who can become certified to maintain the quality of their certified professionals.
Certification Process Overview
The journey to becoming Epic Ambulatory Billing certified typically follows these steps:
- Nomination: Your organization selects you as a candidate for certification.
- Application: Your employer submits your information to Epic for approval.
- E-Learning: Complete online preparatory courses through Epic’s Learning Home portal.
- In-Person Training: Attend classes at Epic’s campus in Verona, Wisconsin (this may be virtual in some cases).
- Certification Exam: Pass a comprehensive test on ambulatory billing processes.
- Project Work: Complete required implementation or maintenance projects.
- Maintenance: Keep your certification active through continuing education.
The entire process usually takes several weeks to a few months, depending on scheduling and your pace through the e-learning components.
Core Components of the Training
Epic Ambulatory Billing Modules
During certification, you’ll learn about several key Epic modules related to outpatient billing:
1. Cadence
While primarily a scheduling system, Cadence affects billing by capturing:
- Patient appointment information
- Insurance verification details
- Copay collection opportunities
- Check-in and registration data
Understanding this module helps you see how the revenue cycle begins with the patient’s first contact.
2. Prelude/Registration
This module handles patient registration, which is critical for billing because it:
- Verifies patient demographics
- Captures insurance information
- Establishes guarantor relationships
- Creates the foundation for clean claims
Errors at this stage can lead to major billing problems down the line.
3. Resolute Professional Billing (PB)
This is the core billing module you’ll spend most time learning about. It handles:
- Charge entry and claim creation
- Payment posting and adjustments
- Denial management
- Collection workflows
- Financial reporting
Mastering Resolute PB is essential for the certification.
4. Reporting Workbench
This tool allows you to create and run reports to:
- Track billing performance
- Identify bottlenecks in revenue cycle
- Monitor claim status
- Analyze financial trends
Learning to use these reports effectively is a key part of the certification.
Key Workflows and Processes
The certification training covers essential workflows that ambulatory billers need to understand:
- Charge Entry: How charges are created, either manually or automatically, and how to review them for accuracy.
- Claim Creation: The process of bundling charges into claims and submitting them to insurance companies.
- Payment Posting: How to correctly apply payments received from patients and insurers.
- Denial Management: Procedures for identifying, tracking, and resolving denied claims.
- Patient Billing: Methods for generating statements and managing patient financial responsibility.
- Month-End Closing: Steps for reconciling accounts at the end of each financial period.
For each workflow, you’ll learn both the technical steps in Epic and the best practices that ensure efficient operations.
Practical Training Elements
Hands-On Exercises
A significant portion of the certification training involves practical exercises in a test environment. These exercises help you:
- Practice real-world scenarios you’ll face on the job
- Learn keyboard shortcuts that increase efficiency
- Understand how different parts of the system connect
- Develop troubleshooting skills for common issues
These exercises often simulate typical clinic situations, such as:
- Processing a visit from check-in through final payment
- Correcting errors on claims that were rejected
- Running financial reports and analyzing the results
- Setting up common billing workflows
System Configuration Skills
Beyond just using Epic, the certification teaches you how to customize certain aspects of the system:
- Creating letter templates for patient communications
- Setting up work queues for efficient task management
- Customizing claim scrubber rules to catch errors
- Designing personalized workspace layouts
These configuration skills help you adapt Epic to your specific clinic’s needs and increase overall efficiency.
Certification Exam Details
Exam Format and Content
The Epic Ambulatory Billing certification exam typically:
- Takes 2-3 hours to complete
- Contains multiple-choice questions
- Includes scenario-based problems
- Requires practical demonstrations in the system
- Covers all major ambulatory billing workflows
The exam tests both your theoretical knowledge and practical abilities to use the system correctly.
Study Tips and Preparation Strategies
To succeed on the certification exam, experienced professionals recommend:
- Take thorough notes during training sessions and e-learning modules.
- Practice in the playground environment as much as possible before the exam.
- Create flashcards for key concepts, workflows, and system locations.
- Form study groups with colleagues pursuing the same certification.
- Teach concepts to others, which helps solidify your own understanding.
- Focus on troubleshooting skills, as the exam often asks how you would solve common problems.
- Get plenty of rest before exam day to ensure you’re mentally sharp.
Common Challenges and How to Overcome Them
Many candidates struggle with these aspects of certification:
- System navigation speed: Practice using keyboard shortcuts instead of mouse clicks.
- Understanding the billing cycle holistically: Create diagrams that show how each step connects to the next.
- Remembering specific file locations: Create mnemonic devices or visual maps of the system structure.
- Connecting technical steps to business reasons: For each process you learn, ask “why is this important?”
Benefits of Becoming Certified
Career Advantages
Epic Ambulatory Billing Certification can significantly boost your career in healthcare:
- Higher salary potential: Certified professionals often earn 15-20% more than non-certified peers.
- Job security: Organizations rarely let go of Epic-certified staff due to the investment in their training.
- Promotion opportunities: Certification often leads to leadership roles in revenue cycle departments.
- Internal mobility: You become valuable across different departments that deal with billing.
- External opportunities: Other healthcare organizations using Epic may recruit you for your expertise.
Organizational Benefits
For healthcare organizations, having Epic Ambulatory Billing certified staff members provides:
- Reduced dependence on consultants, saving thousands of dollars in external support costs.
- Improved revenue capture through more accurate and efficient billing processes.
- Faster claim payments due to cleaner submissions and fewer rejections.
- Better ability to adapt to changing healthcare payment models.
- Internal training resources who can help other staff learn the system.
Maintaining Your Certification
Continuing Education Requirements
Epic requires certified professionals to keep their knowledge current through:
- Quarterly updates: Brief online modules about system changes and new features.
- Annual assessments: Short tests to verify continued competency.
- Version upgrades: Additional training when major system versions are released.
- Proficiency demonstrations: Occasional projects to show you’re using the system correctly.
Failing to complete these requirements can result in your certification becoming inactive.
Best Practices for Long-Term Success
To maintain not just your certification but your expertise as an Epic Ambulatory Billing specialist:
- Join Epic’s online community to stay connected with other users and keep up with discussions.
- Attend Epic’s User Group Meetings (UGM) when possible to learn from other organizations.
- Volunteer for pilot projects at your organization to get early exposure to new features.
- Create a knowledge repository of solutions to unusual problems you encounter.
- Mentor newer users to reinforce your own knowledge while helping others.
- Stay informed about healthcare billing regulations to understand the “why” behind system updates.
Advanced Knowledge and Specialization
Related Epic Certifications
After mastering Ambulatory Billing, you might consider these related Epic certifications:
- Hospital Billing: Extends your knowledge to inpatient billing workflows.
- Claims: Focuses specifically on the claims creation and management process.
- Revenue Guardian: Specializes in preventing revenue leakage through system monitoring.
- Reporting: Develops advanced skills in creating and analyzing financial reports.
Each additional certification makes you more valuable to your organization and more marketable in your career.
Becoming a Subject Matter Expert
The most successful Epic Ambulatory Billing certified professionals often become subject matter experts (SMEs) who:
- Lead system optimization initiatives
- Train and support other staff members
- Represent the billing department in system discussions
- Help translate between technical and operational teams
- Contribute to strategic decisions about revenue cycle management
This role requires not just system knowledge but also strong communication skills and broad understanding of healthcare finance.
Common Epic Ambulatory Billing Challenges
Technical Issues and Workarounds
Even experienced users face challenges with Epic’s billing system. Here are common issues and solutions:
- Charge Routing Problems
- Issue: Charges get stuck in queues and don’t move forward.
- Solution: Check routing rules configurations and user security settings.
- Claim Rejection Patterns
- Issue: Similar claims repeatedly get rejected.
- Solution: Create claim edit rules to catch problems before submission.
- Report Performance
- Issue: Critical reports run slowly during busy periods.
- Solution: Schedule reports to run during off-hours and save results.
- System Slowdowns
- Issue: Processing becomes sluggish during month-end.
- Solution: Coordinate with IT to optimize database performance during busy periods.
Integration with Other Epic Modules
Ambulatory Billing doesn’t exist in isolation. Certified specialists need to understand how it connects with:
- MyChart: Patient portal payments and statement delivery
- Referrals: Authorization tracking that affects claim approval
- Clinical Systems: Documentation that supports medical necessity
- Healthy Planet: Population health initiatives that may have alternative payment models
Understanding these connections helps resolve issues that cross module boundaries.
The Future of Epic Ambulatory Billing
Emerging Trends and Updates
Epic’s ambulatory billing system continues to evolve. Current trends include:
- AI-Assisted Coding: Machine learning tools that suggest appropriate billing codes based on documentation.
- Patient Financial Experience Enhancements: Tools that make billing more transparent and easier for patients to understand.
- Value-Based Care Support: Features that help track quality measures that affect reimbursement.
- Mobile Capabilities: Expanded options for managing billing tasks from smartphones and tablets.
- Telehealth Integration: Improved billing workflows for virtual visits, which have become permanent fixtures in healthcare.
Preparing for System Evolution
To stay ahead as Epic’s system changes:
- Pay attention to quarterly update notes from Epic
- Participate in pre-release testing when possible
- Join special interest groups focused on revenue cycle
- Connect with Epic’s billing specialists at conferences
- Share challenges and solutions with other organizations
Real-World Success Stories
Case Study: Optimizing Claim Submission
A large medical group with Epic Ambulatory Billing certified staff was able to:
- Reduce claim rejection rates from 12% to under 3%
- Decrease average days in accounts receivable from 45 to 28 days
- Increase clean claim rate to 97%
- Improve first-pass payment rate by 22%
They achieved this by leveraging the advanced knowledge their certified staff had about Epic’s claim scrubber rules and work queue management.
Case Study: Patient Payment Improvements
A multi-specialty clinic used their Epic-certified billing team to:
- Implement point-of-service collections that increased upfront payments by 35%
- Create custom payment plans that reduced bad debt by 18%
- Design patient-friendly statements that improved self-pay collection rates
- Set up automated payment reminder workflows that decreased staff phone time
These improvements were possible because certified staff understood both the technical capabilities of Epic and the patient billing experience.
Conclusion
Epic Ambulatory Billing Certification represents a significant investment in your healthcare career. It validates your expertise in managing outpatient billing workflows within one of healthcare’s most widely-used electronic health record systems.
The certification process is rigorous, combining technical system knowledge with practical billing expertise. However, the benefits both for individual careers and healthcare organisations make it well worth the effort.
For healthcare professionals interested in the business side of medicine, this certification opens doors to stable, well-compensated positions with clear paths for advancement. As healthcare continues to evolve, the specialized knowledge of Epic-certified professionals will remain in high demand, particularly as organizations focus on optimizing revenue in an increasingly complex payment landscape.
Whether you’re considering pursuing this certification yourself, hiring certified professionals, or working alongside them, understanding the depth and value of this credential helps appreciate the critical role these specialists play in maintaining the financial health of ambulatory care organizations.