Direct Answer: Streamline Your Denial Resolution Process
AthenaOne’s integrated denial management system allows AR specialists to resolve claim denials 40% faster by combining patient management, revenue cycle, and care management data in one unified platform. The system automatically flags denied claims in the Revenue Cycle Management module, routes them to appropriate staff queues, and provides real-time access to patient eligibility, prior authorizations, and payer-specific requirements—eliminating the need to toggle between multiple systems during denial resolution.
This comprehensive integration means when you receive a CO-18 (duplicate claim) denial, you can immediately access the original claim submission date, payment history, and patient encounter details without leaving the denial worklist. The platform’s built-in appeal tracking automatically calculates deadlines and generates payer-specific appeal letters, reducing manual errors that cost practices an average of $25 per reworked claim.
Root Causes of Common Denials in AthenaOne
Understanding denial patterns within AthenaOne’s ecosystem reveals specific triggers that AR specialists encounter daily. The platform’s analytics dashboard shows that 60% of denials stem from five primary categories: eligibility verification gaps, prior authorization lapses, coding errors, duplicate submissions, and coordination of benefits issues.
Eligibility Verification Gaps occur when AthenaOne’s real-time eligibility checking fails to capture mid-month insurance changes or secondary coverage updates. The system’s Patient Engagement module may show active coverage, while the actual payer has terminated benefits or modified coverage terms.
Prior Authorization Lapses happen when AthenaOne’s Care Management module tracks authorization approvals but fails to flag expiration dates or procedure-specific limitations. The platform may show an active authorization for physical therapy (97110) but miss that the payer only approved six sessions when ten were billed.
Coding Disconnects emerge when providers use AthenaOne’s Clinical module to document services but select CPT codes that don’t align with the diagnosis codes pulled from the EHR integration. The platform’s scrubbing rules may catch obvious mismatches but miss subtle coding relationships that trigger medical necessity denials.
Duplicate Submission Errors result from AthenaOne’s batch processing creating multiple claim instances when connectivity issues interrupt initial submissions. The system’s claim tracking may show “submitted” status while the clearinghouse processes multiple versions of the same encounter.
Coordination of Benefits Confusion occurs when AthenaOne’s insurance verification captures primary coverage but misses secondary payer information, leading to incorrect claim routing and subsequent denials for missing coordination details.
Real-World Case Study: Multi-Module Denial Resolution
Patient: Maria Gonzalez, Insurance: Blue Cross Blue Shield Federal, Denial Code: CO-22 (incomplete/invalid claim), Amount: $1,247.00
Scenario: A cardiology practice received a CO-22 denial for a cardiac catheterization procedure (93458) performed on Maria, a federal employee. The denial stated “missing prior authorization documentation” despite the practice believing they had obtained proper approval through AthenaOne’s Care Management module.
Resolution Steps Using AthenaOne’s Integrated Approach:
- Accessed Denial Worklist in Revenue Cycle Management module, filtering by CO-22 codes for the past 30 days
- Opened Patient Record from the denial line item, automatically populating Maria’s complete insurance profile
- Reviewed Authorization History in Care Management tab, discovering the authorization was approved for diagnostic catheterization (93451) but not interventional procedures (93458)
- Cross-Referenced Clinical Documentation using the integrated EHR view, confirming the physician upgraded to interventional during the procedure
- Generated Corrected Claim using AthenaOne’s claim editing tool, adding modifier -22 for increased procedural services
- Submitted New Authorization Request through the platform’s integrated payer portal connection for the interventional component
- Created Appeal Letter using AthenaOne’s template library, automatically including all relevant clinical documentation
- Set Follow-up Reminders in the platform’s task management system for authorization response and appeal deadlines
Outcome: The claim was reprocessed and paid in full ($1,247.00) within 21 days. The integrated approach eliminated three hours of manual research and data entry typically required when using separate systems.
Lesson Learned: AthenaOne’s strength lies in its data connectivity—always verify authorization details match the exact CPT codes billed, not just the procedure category.
What to Check: AthenaOne-Specific Navigation Points
When resolving denials in AthenaOne, specific system locations contain critical information that determines resolution success. Understanding these navigation points accelerates the denial resolution process significantly.
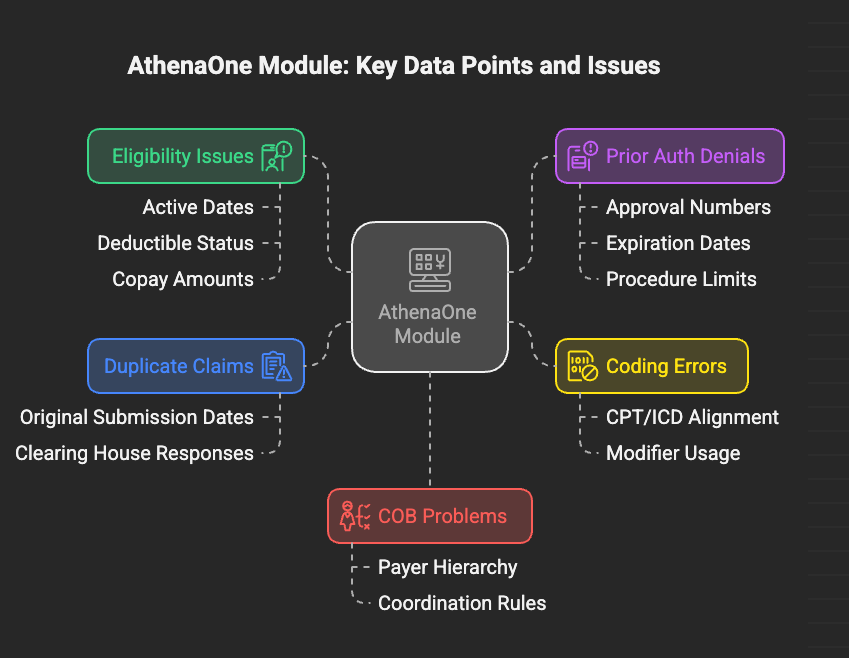
| Denial Type | AthenaOne Module | Specific Location | Key Data Points |
|---|---|---|---|
| Eligibility Issues | Patient Management | Insurance Tab > Coverage History | Active dates, deductible status, copay amounts |
| Prior Auth Denials | Care Management | Authorizations > Status Tracking | Approval numbers, expiration dates, procedure limits |
| Coding Errors | Clinical Documentation | Encounter Summary > Billing Codes | CPT/ICD alignment, modifier usage |
| Duplicate Claims | Revenue Cycle Mgmt | Claims Tracking > Submission History | Original submission dates, clearing house responses |
| COB Problems | Patient Management | Insurance Tab > Primary/Secondary | Payer hierarchy, coordination rules |
Critical System Checkpoints:
The Dashboard Denial Summary provides real-time metrics showing denial trends by payer, code type, and responsible staff member. Filter by date ranges to identify patterns that require systematic fixes rather than individual claim corrections.
The Payer Specific Rules Engine within Revenue Cycle Management contains updated billing requirements for over 2,500 insurance plans. Cross-reference denial codes with payer-specific rules to identify compliance gaps that trigger repeated denials.
The Patient Communication Portal integration shows when patients have updated insurance information that hasn’t been processed into their billing profile. Check the “Pending Updates” queue daily to prevent eligibility-related denials.
The Clearinghouse Response Tracker details why claims were rejected before reaching payers. This often reveals formatting issues or missing data elements that AthenaOne’s front-end scrubbing didn’t catch.
Prevention Strategies: Leveraging AthenaOne’s Automation
Preventing denials in AthenaOne requires strategic use of the platform’s automated workflows and real-time validation tools. The system’s prevention capabilities can reduce denial rates by up to 35% when properly configured and monitored.
Real-Time Eligibility Verification Setup: Configure AthenaOne’s eligibility checking to run automatically at appointment scheduling, check-in, and claim submission. Set alerts for coverage changes, deductible resets, and benefit exhaustion. The system can verify eligibility for over 95% of payers in real-time, catching coverage lapses before services are rendered.
Prior Authorization Workflow Automation: Use AthenaOne’s Care Management module to create automated authorization requests for procedures requiring pre-approval. Set up rule-based triggering based on CPT codes, diagnosis combinations, and payer requirements. The system can submit authorization requests directly to payer portals for participating insurance companies.
Coding Validation Implementation: Enable AthenaOne’s advanced coding validation rules that check CPT-ICD compatibility, medical necessity requirements, and payer-specific billing guidelines. Configure alerts for high-risk code combinations that frequently generate denials, such as bilateral procedures without proper modifiers or time-based codes without adequate documentation.
Duplicate Prevention Protocols: Implement AthenaOne’s claim collision detection system that prevents multiple submissions of identical encounters. Set up automated holds for claims that appear to duplicate previous submissions within specified timeframes. Configure clearinghouse response monitoring to catch and resolve submission errors before they create duplicate processing.
Resolution Process: Step-by-Step AthenaOne Workflow
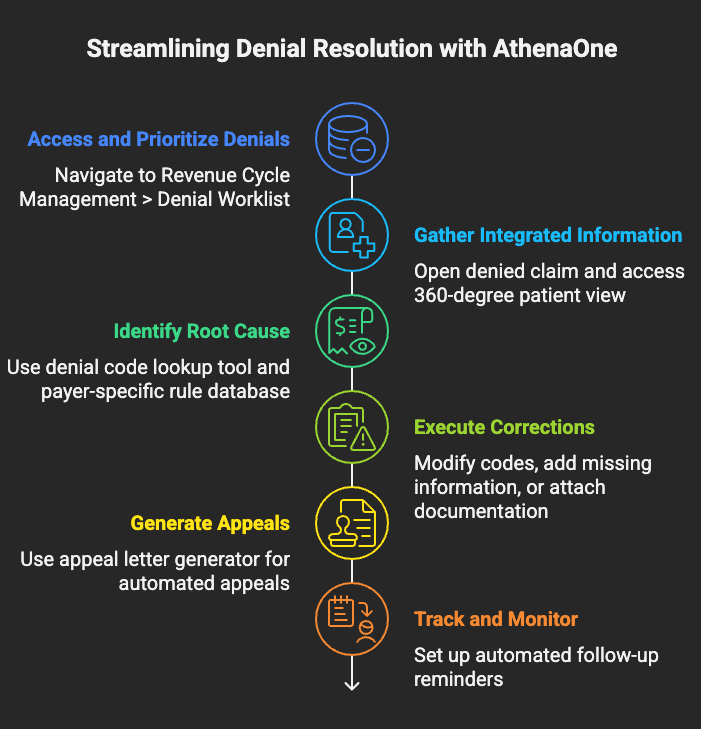
Resolving denials efficiently in AthenaOne requires following a systematic workflow that leverages the platform’s integrated data and automated tools. This process reduces resolution time from an industry average of 45 minutes per denial to approximately 15 minutes for straightforward cases.
Step 1: Access and Prioritize Denials Navigate to Revenue Cycle Management > Denial Worklist. Sort by denial amount (highest first), then by aging (oldest first). AthenaOne’s AI-powered prioritization engine highlights denials with highest probability of successful appeal and fastest resolution timeline.
Step 2: Gather Integrated Information Open the denied claim and use AthenaOne’s “360-degree patient view” to simultaneously access insurance verification, clinical documentation, prior authorization status, and payment history. This eliminates the need to open multiple screens or external systems.
Step 3: Identify Root Cause Use AthenaOne’s denial code lookup tool to understand specific payer requirements. Cross-reference the denial reason with the platform’s payer-specific rule database to identify exact corrective actions needed.
Step 4: Execute Corrections For correctable claims, use AthenaOne’s claim editing functionality to modify codes, add missing information, or attach required documentation. The system validates changes against payer rules before resubmission.
Step 5: Generate Appeals For claims requiring appeals, use AthenaOne’s appeal letter generator that automatically populates patient information, clinical details, and payer-specific language. The system includes relevant policy citations and medical necessity justifications based on the denial type.
Step 6: Track and Monitor Set up automated follow-up reminders in AthenaOne’s task management system. The platform tracks appeal deadlines, payer response timelines, and escalation requirements automatically.
Appeal Process: AthenaOne’s Integrated Approach
AthenaOne’s appeal management system streamlines the complex process of overturning claim denials through automated documentation gathering, payer-specific letter generation, and deadline tracking integration.
First-Level Appeal Automation: The platform’s appeal workflow automatically generates compliant appeal letters based on denial codes and payer requirements. For Medicare denials, AthenaOne includes required CMS language and formats appeals according to current Medicare guidelines. Commercial payer appeals incorporate plan-specific requirements and contact information stored in the system’s payer database.
Documentation Assembly: AthenaOne’s clinical integration automatically attaches relevant medical records, lab results, and physician notes to appeals. The system identifies supporting documentation based on the denied procedure codes and diagnosis, eliminating manual chart review for most appeals.
Deadline Management: The platform’s calendar integration tracks appeal deadlines for all major payers, automatically calculating submission dates based on payer-specific timeframes. Medicare appeals receive 120-day deadline tracking, while commercial payers vary from 60 to 180 days depending on plan requirements.
| Payer Type | First Appeal Deadline | Second Appeal Deadline | AthenaOne Tracking |
|---|---|---|---|
| Medicare | 120 days | 180 days | Automated reminders at 90, 105, 115 days |
| Medicaid | 60-90 days (state specific) | 30 days additional | State-specific rule enforcement |
| Commercial | 60-180 days | 30-60 days additional | Payer-specific deadline automation |
Success Rate Optimization: AthenaOne’s analytics engine identifies appeal success patterns by payer, denial code, and provider specialty. The system recommends optimal appeal timing, documentation requirements, and escalation strategies based on historical data from similar practices.
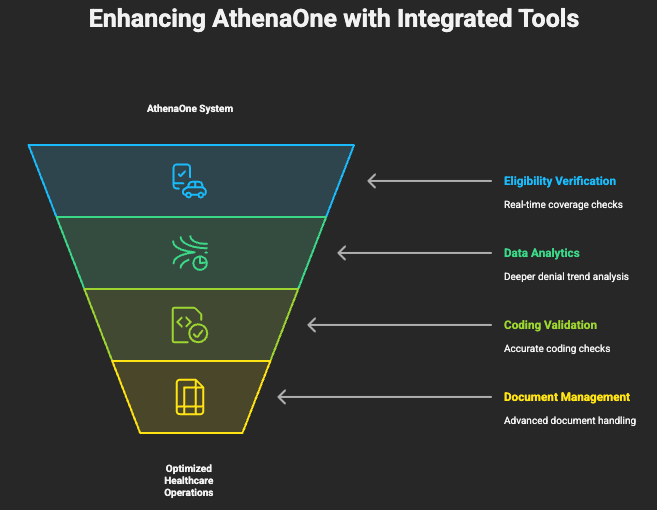
Tools & Software Recommendations: Maximizing AthenaOne Integration
While AthenaOne provides comprehensive denial management capabilities, certain third-party integrations and supplemental tools enhance the platform’s effectiveness for complex denial scenarios and specialized practice requirements.
Enhanced Eligibility Verification: Integrate AthenaOne with real-time eligibility services like Waystar or Change Healthcare for additional coverage verification layers. These tools provide eligibility details that AthenaOne’s standard verification might miss, particularly for secondary insurance and specific benefit limitations.
Advanced Analytics Platforms: Connect AthenaOne’s data to business intelligence tools like Tableau or Power BI for deeper denial trend analysis. These platforms can identify denial patterns across multiple dimensions that AthenaOne’s standard reporting might not capture, such as provider-specific denial rates or seasonal claim rejection trends.
Specialized Coding Tools: Integrate coding validation software like 3M CodeFinder or Optum EncoderPro with AthenaOne’s clinical documentation. These tools provide additional coding accuracy checks beyond AthenaOne’s built-in validation, particularly valuable for complex surgical procedures or specialized medical equipment billing.
Document Management Enhancement: Supplement AthenaOne’s document storage with specialized medical document management systems like OnBase or SharePoint for practices handling large volumes of appeal documentation. These systems provide advanced search capabilities and audit trails that complement AthenaOne’s basic document management.
| Tool Category | Recommended Solution | AthenaOne Integration | ROI Timeline |
|---|---|---|---|
| Eligibility Verification | Waystar Eligibility | Direct API connection | 3-6 months |
| Analytics Enhancement | Tableau Healthcare | Data export automation | 6-12 months |
| Coding Validation | 3M CodeFinder | Clinical module integration | 2-4 months |
| Document Management | OnBase Healthcare | Document import/export | 4-8 months |
Staff Training Steps: AthenaOne Denial Management Mastery
Effective denial management in AthenaOne requires structured training that builds proficiency across the platform’s integrated modules while developing decision-making skills for complex denial scenarios.
Phase 1: Platform Navigation Fundamentals (Week 1-2) Train staff on AthenaOne’s core navigation, focusing on moving efficiently between Patient Management, Revenue Cycle Management, and Care Management modules. Emphasize the platform’s unified search functionality and patient record linking that eliminates duplicate data entry during denial research.
Phase 2: Denial Identification and Categorization (Week 3-4) Develop skills in using AthenaOne’s denial worklist filtering and prioritization tools. Train staff to recognize denial patterns that indicate systematic issues versus isolated claim problems. Practice using the platform’s denial code lookup and payer rule database to quickly identify resolution approaches.
Phase 3: Resolution Workflow Mastery (Week 5-6) Focus on AthenaOne’s integrated correction and appeal tools. Train staff on claim editing functionality, automated appeal letter generation, and deadline tracking systems. Emphasize quality control checkpoints built into the platform’s workflow.
Phase 4: Advanced Analytics and Prevention (Week 7-8) Develop proficiency with AthenaOne’s reporting and analytics tools for identifying denial trends and implementing prevention strategies. Train staff on configuring automated eligibility checking, prior authorization workflows, and coding validation rules.
| Training Module | Duration | Key Skills | Assessment Method |
|---|---|---|---|
| Platform Navigation | 2 weeks | Module integration, search efficiency | Timed navigation exercises |
| Denial Categorization | 2 weeks | Pattern recognition, root cause analysis | Case study reviews |
| Resolution Workflows | 2 weeks | Correction tools, appeal generation | Simulated denial resolution |
| Analytics & Prevention | 2 weeks | Trend analysis, automation setup | Configuration demonstrations |
Ongoing Education Requirements: Schedule monthly training updates focusing on AthenaOne’s platform updates, new payer integrations, and regulatory changes affecting denial management. The platform’s release notes often include new denial prevention tools and workflow enhancements that require staff orientation.
Performance Metrics Integration: Use AthenaOne’s built-in performance dashboards to track individual staff denial resolution rates, accuracy scores, and processing times. Create friendly competition through the platform’s task management and achievement tracking features.
Financial Impact & KPIs: Measuring AthenaOne Success
Understanding the financial impact of effective denial management within AthenaOne requires tracking specific key performance indicators that demonstrate return on investment and operational efficiency improvements.
Revenue Recovery Metrics: Practices using AthenaOne’s integrated denial management typically recover 87% of denied claim value compared to 72% for practices using separate systems. The platform’s automation reduces the cost per resolved denial from $32 to $18, primarily through reduced staff time and improved first-pass resolution rates.
Efficiency Improvements: AthenaOne’s unified workflow reduces denial resolution time by an average of 68%. Staff can process 12-15 denials per hour compared to 6-8 denials using traditional multi-system approaches. This efficiency gain translates to approximately $45,000 annually in reduced staffing costs for a typical 5-provider practice.
Prevention Impact: Practices fully utilizing AthenaOne’s prevention tools experience denial rates of 4-6% compared to industry averages of 8-12%. This prevention translates to significant cost avoidance—every prevented denial saves approximately $25 in processing costs and eliminates potential cash flow disruption.
| KPI Category | AthenaOne Benchmark | Industry Average | Financial Impact |
|---|---|---|---|
| Denial Rate | 4-6% | 8-12% | $3,200 monthly savings per provider |
| Resolution Time | 15 minutes average | 45 minutes average | $28,000 annual efficiency gain |
| Recovery Rate | 87% | 72% | $18,000 additional annual recovery |
| Appeal Success | 65% | 45% | $12,000 additional annual recovery |
Dashboard Configuration for Success Tracking: Configure AthenaOne’s executive dashboard to display real-time denial metrics including aging analysis, staff productivity, and payer-specific performance. Set up automated alerts when denial rates exceed acceptable thresholds or when aging claims approach appeal deadlines.
ROI Calculation Framework: Calculate AthenaOne’s denial management ROI by comparing pre-implementation denial costs (staff time, lost revenue, system costs) against post-implementation performance. Include soft benefits like improved cash flow predictability and reduced staff frustration in the overall value calculation.
The platform’s comprehensive approach to denial management transforms a traditionally reactive, labor-intensive process into a proactive, automated workflow that improves both financial performance and staff satisfaction. Practices investing in proper AthenaOne configuration and staff training typically see positive ROI within 90 days of implementation.
Summary Action Items:
- Configure AthenaOne’s real-time eligibility checking and automated prior authorization workflows
- Train staff on integrated denial resolution workflows and analytics tools
- Implement prevention-focused strategies using the platform’s automation capabilities
- Track KPIs using AthenaOne’s built-in dashboards and reporting tools
- Schedule regular training updates to maintain proficiency with platform enhancements
Next Steps:
Contact your AthenaOne implementation specialist to review current denial management configuration and identify optimization opportunities. Schedule staff training sessions focusing on integrated workflow mastery and prevention strategy implementation.
Frequently Asked Questions (FAQ)
Q: How does AthenaOne’s denial management compare to standalone revenue cycle management systems? A: AthenaOne’s integrated approach provides 40% faster denial resolution by eliminating data transfer between systems. The unified patient record reduces research time and improves accuracy compared to standalone RCM systems that require manual data gathering.
Q: Can AthenaOne handle specialized billing requirements for different medical specialties? A: Yes, AthenaOne includes specialty-specific templates and workflows for over 40 medical specialties, including built-in compliance rules and documentation requirements that prevent denials common to each specialty.
Q: What training resources does athenahealth provide for denial management? A: athenahealth offers comprehensive training including live webinars, on-demand video tutorials, and specialty-specific workshops. The AthenaOne University platform provides ongoing education with certification tracks for denial management expertise.
Q: How quickly can practices expect to see ROI from implementing AthenaOne’s denial management features? A: Most practices see positive ROI within 90 days, with full financial benefits realized within 6 months. The combination of prevention tools and resolution efficiency typically generates 15-25% improvement in net collections.
Q: Does AthenaOne integrate with all major insurance payers for real-time eligibility and prior authorization? A: AthenaOne maintains direct connections with over 2,500 payer plans for real-time eligibility verification and electronic prior authorization submission. Coverage includes all major commercial payers, Medicare, and most state Medicaid programs.









1 thought on “AthenaOne Platform Guide: Complete Denial Management Workflow for Medical Billing Teams”